Millions of people everywhere would literally jump and down if there was a pill that would get rid of the unsightly veins that appear and seemingly crawl over your legs. Unfortunately it’s just not that easy. Varicose veins can develop when leg veins aren’t strong enough to pump the blood back up to your heart. As a result, blood begins to pool in your legs. The remedies I suggest at the end of the article may be able to not only support healthy veins and circulation, but also relieve the pain experienced from hemorrhoids (varicose veins in the wall of the rectum and anus) as well. Let’s begin our discussions about varicose veins.
What Are Varicose Veins?
Varicose veins are twisted or gnarled veins that have become abnormally enlarged. Also known as varicosities, these veins are named after the Latin root word “varix,” which means “twisted.” They are sometimes described as lumpy, winding vessels that are visible immediately below the surface of the skin. While any vein can become varicose, it happens most often to the veins of the legs and feet, mainly due to the effects of gravity in the lower parts of the body. There are three types of veins: superficial veins (found just below the surface), deep veins (larger vessels inside the muscles), and perforator veins(connecting the superficial and deep veins). Most varicosities take place in the superficial veins. The condition of varicose veins is a progressive disease that gets worse over time if there is no intervention.
Varicose veins are fairly common in the United States. It is estimated that approximately 15% of men and 25% of women are affected. This condition can be strictly a cosmetic problem for some individuals, due to their unsightly appearance. Other cases can result in pain and discomfort, and may in some instances lead to more serious complications. Varicose veins can also be an indicator of increased risk for other types of circulatory problems.
What Causes Varicose Veins?
Just in case you haven’t recently reviewed your basic knowledge of the circulatory system, let’s bring you back up to speed in order to better understand how varicose veins occur. Your blood vessels are composed of two major types: arteries, which carry oxygen-rich blood away from the heart to the body’s organs, and veins, which are the vehicle for the blood to flow back to the heart and get replenished with oxygen and nutrients. The veins of the feet and legs have a unique challenge: they must accomplish the task of circulating the blood while working against the force of gravity. When the heart pumps, the blood pressure temporarily increases. Between heartbeats, there is a drop in blood pressure. During this period, blood must resist the pull of gravity. In order to accomplish this, the body has been designed with a series of valves in the veins that open and close at appropriate times to facilitate the flow of blood. Malfunction of one of these valves is how varicose veins begin. When one of them fails to close, blood pressure in that section of the vein goes up, and can trigger the failure of adjacent valves. This causes blood to pool in that area, and the walls of the vein to be weakened. This process can result in a chain reaction that in turn causes even more nearby valves to fail. In addition, the affected veins lose their elasticity and begin to swell. The result is the typical appearance of varicose veins. They are usually blue or dark purple in color because the blood is de-oxygenated. They often appear as twisted chords that bulge out from the skin. Varicose veins that are visible on the surface are called primary, and when varicosities form in the deep veins they are known as secondary.
Certain factors increase an individual’s risk for developing varicose veins. The most common ones include:
- Age: As we get older (especially over the age of 40) the valves in our veins tend to break down from wear and tear and interfere with proper circulation. This is the main factor that causes varicose veins to occur.
- Gender: Women have a higher incidence of varicose veins than men. This is likely due to several factors. Hormonal changes during puberty, menstruation, menopause, or pregnancy have a relaxing effect on vein walls. As they lose their elasticity, it becomes easier for the valves in the veins to malfunction. Using synthetic hormone replacement therapy or birth control pills tends to make matters even worse, and will increase a woman’s risk for varicose veins. Another factor is pregnancy itself. The circulatory system adjusts to meet the needs of the fetus by increasing the volume of blood in the body, and at the same time decreasing the amount of blood flowing from the legs to the pelvis. This may result in the onset of new varicosities or the aggravation of existing ones. Hemorrhoids, which are also a common side effect of pregnancy, are actually varicosities of the anal area.
- Heredity: If you have a family history of varicose veins, your chance of developing them is increased. The specifics of how this genetic connection works are not well understood. Also, people with light skin who have experienced high levels of sun exposure and skin damage.
- Obesity: Extra weight puts a strain on every system in our bodies, and the circulatory system is no exception. Being overweight causes the veins to be put under greater pressure, and thus lose their flexibility more easily.
- Inactive lifestyle: Whether it is standing or sitting for long periods of time in a work or other situation, or simply sedentary patterns with little physical activity, insufficient exercise will contribute to a greater risk for varicose veins. As the phrase “get your blood moving” indicates, exercise helps to keep our circulatory systems working properly and efficiently.
- Sitting or Standing for long periods of time: Going for long times without moving around allows blood to pool in the legs and slows down blood flow.
- Pregnancy or women who have recently given birth.
- Hormonal Changes or Imbalances: Especially peri-menopausal and post-menopausal women; teens going through puberty and women who are using synthetic birth control.
What Are the Symptoms of Varicose Veins?
Many times varicose veins are just an eyesore that folks would rather do without, especially in the early stages. With some individuals, they never progress beyond that. However, it is not uncommon for patients to experience more significant symptoms. These may include the following:
- Pain of various types, usually in the legs. The pain or discomfort may take the form of aching, or a feeling of heaviness or bloatedness in the legs. Some folks also experience swelling, throbbing, burning, or muscle cramps such as “Charlie horses.”
- Itching around the affected veins is also common, and can be very intense in some cases.
- The dark bulging chords that are characteristic of varicose veins most often make their appearance on the inside of the legs or the backs of the calves. However, they can form anywhere from your ankles to your groin.
- Spider veins, or spider-burst veins, as they are sometimes called, are very small varicose veins that often appear on the face as well as the legs. They can be red or blue, and look similar to a spider’s web or the branches of a tree. They are frequently associated with pregnancy.
What Complications Can Result From Varicose Veins?
Untreated varicose veins will naturally progress in most people, and become larger and more obvious. Symptoms will also tend to worsen over time. Beyond these factors, there are two main possible complications to be aware of: ulcers and edema.
- Open sores or ulcers may form in some varicosity patients, typically found near the ankles. The tissues essentially become “water-logged,” so to speak. These can be very painful for some people, and are the result of abnormally high blood pressure in the veins of the affected area. A common warning sign that precedes the ulcers is brownish discoloration of the skin. The development of these ulcers is a potentially dangerous situation that should be dealt with promptly.
- When deep veins develop varicosities, a condition known as edema can occur. This involves swelling of the leg or legs that have varicose veins. The edema itself can become an issue, but in addition it can point to an even worse problem: the possible presence of a blood clot, a condition known as thrombophlebitis. A blood clot can be life threatening, and demands immediate medical attention.
What Treatments Are Available for Varicose Veins?
There are many options for the treatment or removal of varicose veins. A word of caution is definitely in order here. Since a lot of the possible remedies are for the purpose of cosmetic improvements for the patient, and not considered medically necessary, many of them are not covered by insurance. If you are considering any of the many options for treatment of varicose veins, I suggest you first investigate to see how much they will cost, and secondly verify if they are going to be picked up by your insurance company or must be paid out of pocket. Also keep in mind that many of these procedures are fairly new on the scene, and don’t have much of a track record to measure as far as effectiveness or safety. Be sure you also understand that surgery or other possible treatments may take care of existing varicose veins, but they will not prevent others from forming in the future or reduce your tendency to develop new varicose veins. This can only be accomplished by taking steps to change your lifestyle and improve your overall health.
As far as the most common allopathic “solutions” for varicose veins go, they boil down to three main choices, all of them being various surgical procedures. Please get a second or third opinion before undergoing these or any surgeries for that matter:
- Sclerotherapy: This is a process whereby chemicals are injected into the varicose veins in order to scar them and close them off. This is commonly marketed as a rather casual experience that can be done in your doctors office without anesthesia. What they don’t tell you is that if the injections are not done properly, and especially if the technician misses the vein and injects the chemicals into surrounding tissues, necrosis and scarring can occur that can be very devastating and cosmetically much worse than the original varicosities. Allergic reactions to the chemicals are also not uncommon.
- Laser surgery is now used more and more often to treat varicose veins. The advantages of this is that it is “non-invasive” in the sense that no incisions or needles are needed. However, I would make sure that whoever is performing this procedure on you is adequately skilled and experienced.
- Vein stripping is a more traditional form of surgery where long veins are removed via a series of small incisions. Considered minor surgery, it is usually done on an outpatient basis. However, as the saying goes, there is no such thing as “minor surgery.” Especially when anesthesia is involved.
Natural Recommendations to Help with Varicose Veins
There are many effective and practical steps one can take to both treat and prevent varicose veins. However, before using supplements, it’s best to speak with a knowledgeable practitioner who specializes in vein diseases or “phlebology” since varicose veins may indicate bigger problems including heart disease, deep vein thrombosis or venous insufficiency. Specialists also offer procedures that can dramatically improve the appearance of “varicosities” as they are called.
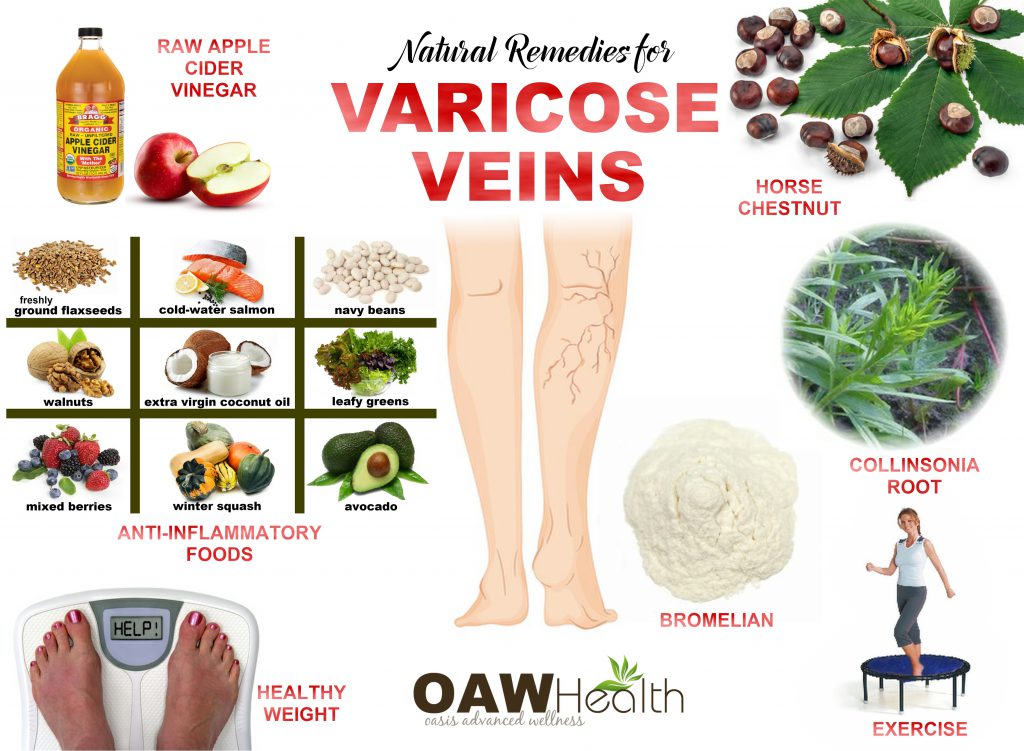
- Exercise – Get up and start moving around! The benefits are countless to your overall health, and are specifically very beneficial to your circulatory system. Physical activities, especially those that involve movement of the legs, strengthen your blood vessels and can prevent varicose veins. Walking, swimming, and biking are excellent choices.
- Healthy Weight – Losing extra pounds can help alleviate existing varicose veins and/or prevent the development of new ones. Eating a low-sodium / high fiber diet is also helpful, as this helps to keep blood pressure down and minimize constipation.
- Loose fitting clothing – Stay away from tight clothing that can interfere with proper circulation. Also avoid high heels ladies. Flats will give your calf muscles a better workout, which is good for your veins.
- Healthy Anti-Inflammatory Diet – Eat foods that are high in fiber; high in Vitamin C and E; natural diuretics such as parsley, cilantro, basil, fennel, dandelion greens, cucumber, asparagus and celery; Spicy foods and herbs such as cayenne, ginger, garlic and onions; Foods rich in magnesium; High Omega-3 fatty acid foods.
- Apple Cider Vinegar – Apple Cider Vinegar (with the mother) improves circulation in the vein walls and is a very effective anti-inflammatory. Many have reported that using ACV along with witch hazel applied on varicose veins can help lower swelling and and improve their appearance within just a few weeks.
- Horse Chestnut – A herbal remedy that has been found to be both effective and safe for helping with varicose veins. Horse Chestnut has also been studied for chronic venous insufficiency that causes pain, ankle swelling, feelings of heaviness, itching and nighttime leg cramping. Horse Chestnut can also help with lowering water retention, circulatory concerns, swelling, diarrhea, PMS cramps and other skin-related issues. Studies have shown that horse chestnut extract provides a similar effect to compression socks and helps to contract veins and arteries. According to the Journal of the Norwegian Medical Association, horse chestnut seed extract is widely used throughout Europe for chronic venous insufficiency (CVI). Italy’s University of Milano performed research that showed aescin to be as effective as compression therapy for CVI and, additionally, aescin is significant for not just CVI, but also hemorrhoids and edema. Why? At the lowest level, horse chestnut seed extract is thought to inhibit the breakdown of capillary wall proteins. Some research has shown that aescin (a compound in Horse Chestnut) is more absorbable by the body during the daytime than night- something to consider if you supplement with horse chestnut.
- Collinsonia Root – Possesses strong anti-oxidant properties. Collinsonia root is known to help with blood flow by alleviating blood vessel contraction, strengthening vein walls, and assisting with the reduction of blood pooling. Those who experience circulatory problems causing them to feel cold all the time, even when the weather is warm, have used this herb to gain relief from chills.
- Bromelain – The enzyme Bromelain breaks down fibrin and promotes better circulation. It has been used in alternative medicine to promote cardiovascular health and to help with hemorrhoids and other conditions of the veins. Bromelain has been suggested to help treat chronic venous insufficiency and may prevent the swelling and soreness caused by varicose veins.
If circulatory health and vein health are an issue in your life, I highly encourage you to find out if there are any things you can change to get your issues under better control. Are you eating a healthy diet full of organic vegetables and fruits? Are you incorporating exercise in your life every day? Would losing some weight put you in better health? When was the last time you cleansed your body? Sometimes these are important factors, but not always. At any rate, if your lifestyle choices aren’t putting you where you want to be, Hematrex® contains organic horse chestnut and is the only vein and circulatory support supplement I recommend.
Research
Horse Chestnut. Natural Center for Complementary and Integrative Health. https://nccih.nih.gov/health/horsechestnut.
Theil, R. Efficacy of glandulars and herbs: the result of 945 cases. The Original Internist. 2012 March. colume 19 (1) 7-11.
Dr. Royal Lee. Collinsonia root (PDF). Standard Process Inc. 1999.
Frostburg.edu. Stoneroot-Collinsonia canadensis L.
H.T. Webster MD, John W. Fyfe MD, J.M. Scudder MD, F.J. Locke MD, H.W. Felter MD. A treatise on Collinsonia candensis. Lloyd Brothers, Pharmacists Inc. 1904.
Stengler, Mark, ND. The Natural Physician’s Healing Therapies: Proven Remedies Medical Doctors Don’t Know. New York, NY: Prentice Hall Press, 2010.
Felixsson E, Persson IA, Eriksson AC, Persson K. Horse chestnut extract contracts bovine vessels and affects human platelet aggregation through 5-HT(2A) receptors: an in vitro study. Phytother Res. 2010 Sep;24(9):1297-301. doi: 10.1002/ptr.3103.
Methlie CB, Schjøtt J. [Horse chestnut–remedy for chronic venous insufficiency]. Tidsskr Nor Laegeforen. 2009 Feb 26;129(5):420-2. doi: 10.4045/tidsskr.09.33871. Norwegian.
Sirtori CR. Aescin: pharmacology, pharmacokinetics and therapeutic profile. Pharmacol Res. 2001 Sep;44(3):183-93. Review.
Suter A, Bommer S, Rechner J. Treatment of patients with venous insufficiency with fresh plant horse chestnut seed extract: a review of 5 clinical studies. Adv Ther. 2006 Jan-Feb;23(1):179-90.
Pittler MH, Ernst E. Horse chestnut seed extract for chronic venous insufficiency. Cochrane Database Syst Rev. 2012 Nov 14;11:CD003230. doi: 10.1002/14651858.CD003230.pub4.
Bässler D, Okpanyi S, Schrödter A, Loew D, Schürer M, Schulz HU. Bioavailability of beta-aescin from horse chestnut seed extract: comparative clinical studies of two Galenic formulations. Adv Ther. 2003 Sep-Oct;20(5):295-304.
†Results may vary. Information and statements made are for education purposes and are not intended to replace the advice of your doctor. Oasis Advanced Wellness/OAWHealth does not dispense medical advice, prescribe, or diagnose illness. The views and nutritional advice expressed by Oasis Advanced Wellness/OAWHealth are not intended to be a substitute for conventional medical service. If you have a severe medical condition or health concern, see your physician of choice.